Medetective
Healthcare,
made accountable.
Medical Fraud Detection
Medetective gives payers, providers, and regulators a single, adaptive lens on claims activity—pinpointing anomalous patterns, flagging suspect encounters in real time, and recommending cost-optimized benefit designs.
By combining OLAP-grade slice-and-dice with machine-learning detection models, it helps the healthcare ecosystem protect funds, improve plan value, and strengthen public trust.
Multidimensional claims cube
OLAP engine aggregates years of claims, eligibility, and provider data; analysts pivot across diagnosis, procedure, geography, and time to uncover hidden cost drivers in seconds.
AI-driven anomaly detection
Adaptive algorithms learn baseline utilisation and instantly surface deviations—up-coding, phantom billing, unbundling, or excessive frequency—reducing manual review queues.
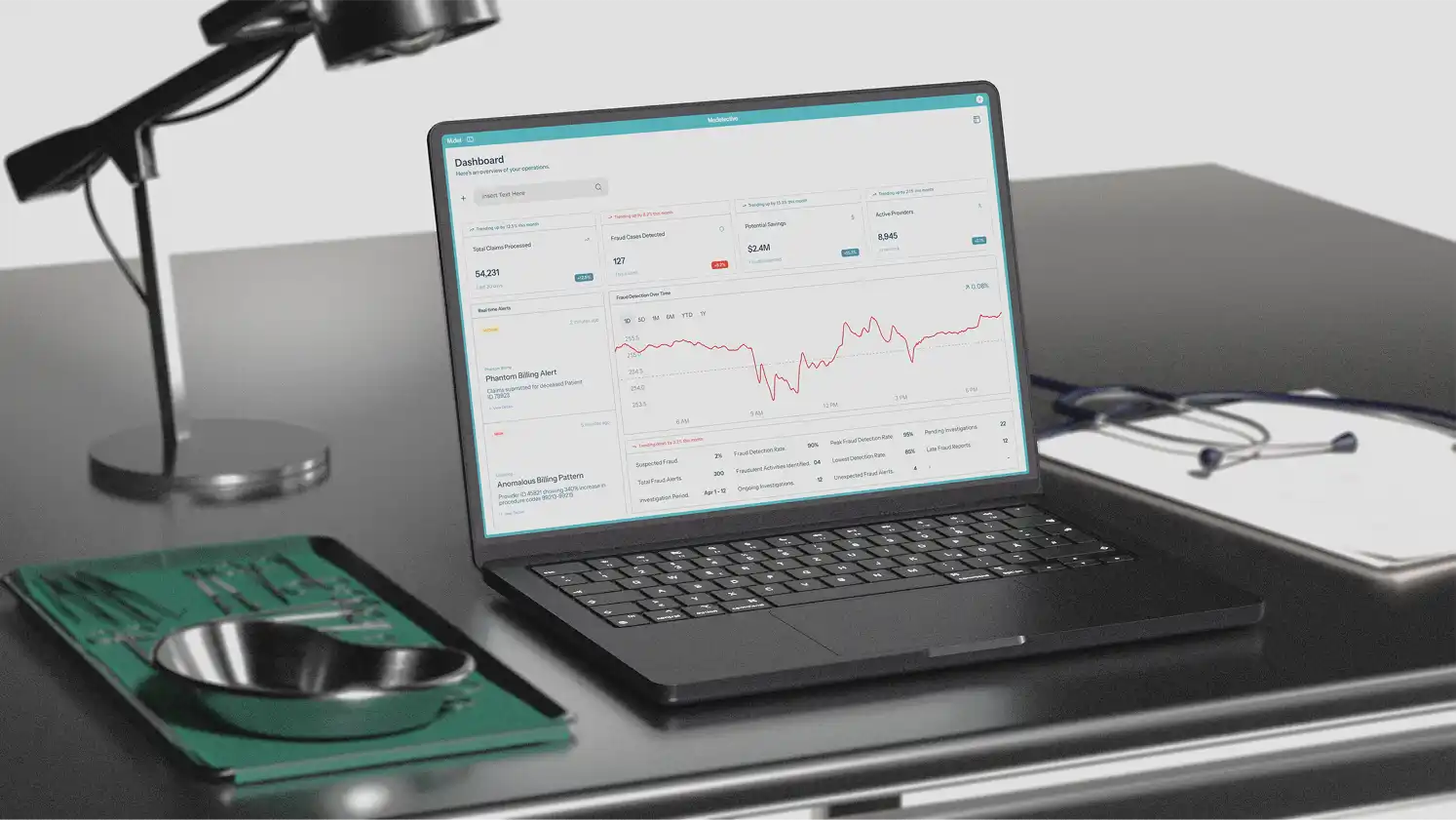
Real-time alerting & dashboards
Streaming analytics push notifications to SIEM, case-management, and mobile apps within milliseconds of a suspicious event, enabling early intervention before payment.
Benefit-package optimiser
Scenario models test deductible, co-pay, and coverage changes against historic utilisation, guiding plan designers toward configurations that curb waste without hurting member satisfaction.
Compliance & audit trail
Immutable logs, role-based access, and exportable evidence packets support HIPAA, GDPR, and insurer-specific audit requirements, preserving chain-of-custody for prosecution.
Scalable, secure deployment
Containerised micro-services run on-prem, private cloud, or sovereign hosting; end-to-end encryption and optional hardware security modules keep PHI under your control as volumes grow.